Over the past two decades, research at the Institute for Work & Health (IWH) and elsewhere has helped shine a light on the importance of various factors on the duration of workers’ compensation claims. But one aspect that has been less well studied is the experience of injured or ill workers after they are no longer receiving services or benefits from the workers’ compensation system.
A research team at IWH has set out to better understand these post-claim experiences. What are workers’ long-term work and health recovery outcomes in the aftermath of an injury or illness? Who are the workers most at risk of having health problems and low job prospects? And what can be done to improve their health and employment outcomes?
“Across the country, few provincial workers’ compensation agencies, worker representatives and employers actually have good answers to these questions,” said Dr. Cameron Mustard, IWH president and senior scientist, in an IWH Speaker Series presentation on early findings from the Ontario Life After Work Injury Study (OLAWIS) cohort. An open access article describing these preliminary findings was also published in September 2021, in BMJ Open (doi:10.1136/bmjopen-2020-048143).
The study is based on interviews with about 1,100 Ontario injured workers. Each was first interviewed 18 months after their work-related injury and then again, if they agreed, 36 months post-injury. The study is designed in part to find out how the post-claim experiences of workers with shorter and longer times on benefit compare, with a particular focus on the experiences of workers who have received benefits or services for more than a year after a disabling injury.
Because this latter group accounts for just six per cent of lost-time claims with Ontario’s Workplace Safety and Insurance Board (WSIB), the research team focused on recruiting such claimants, those with long-duration claims of 12 to 18 months, in roughly equal numbers as claimants with short-duration (between five days and three months) and medium-duration (three to 12 months) claims. (Note that a small number of long-duration study participants would still have had an open claim at the time of the first interview; most, however, did not.)
Changes in employment levels
One of the more notable early findings relates to participants’ return-to-work (RTW) and employment status. The vast majority of workers, ranging from 85 to 93 per cent across the three groups (see table below), did return to work with their injury employer (the employer they were working for when the injury occurred). But 18 months after the injury, a different picture emerged. Although the proportion of workers with the injury employer was roughly equal across the three groups (about 60 per cent), the share of workers not working was much higher among the group with long-duration claims. In addition, the proportion of this group that experienced serious financial difficulties was twice as high as among those with short-duration claims (i.e. those who were back at work within three months).
“This is an example of the important information that's available if lost-time claimants are interviewed after their WSIB benefits or services have ended,” said Mustard.
Differences in self-reported health status were also found across the three groups of claimants. Workers in the long-duration group reported poor or fair health in greater proportions (32.5 per cent versus 16.3 per cent in the short-duration group), had greater sleep issues (49.6 per cent had trouble going to sleep most or all of the time, compared to 33.9 per cent in the short-duration group), and experienced more pain that interfered quite a bit with daily activities (46.0 per cent compared to 18.9 per cent in the short-duration group).
The study also incorporated health-related interview questions from Statistics Canada’s nationally representative Canadian Community Health Survey (CCHS). As a result, the team had an opportunity to compare the health status of the OLAWIS cohort with that of the general population. The team found, for example, that pre-injury levels of diagnosed chronic conditions in the study cohort were generally the same as in the Canadian population. However, following the injury, the prevalence of diagnosis rose markedly in the OLAWIS cohort across several conditions—namely, mood disorders, migraines, back problems and arthritis.
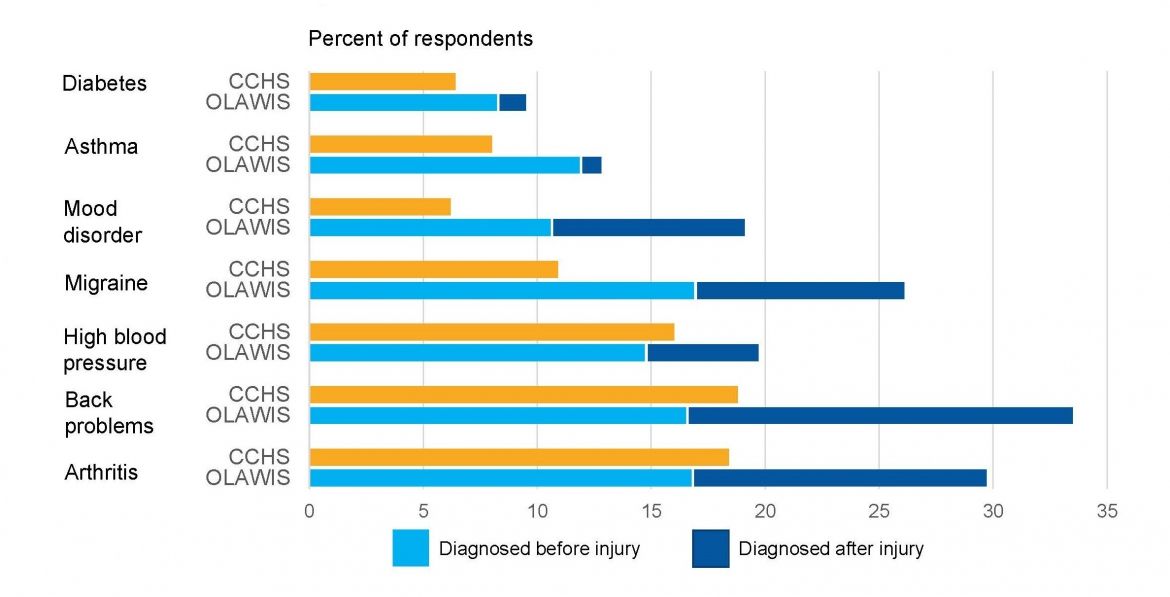
“We can probably attribute a small proportion of this elevated incidence of chronic conditions to enhanced case finding during the clinical treatment of the work-related injury or illness,” said Mustard. “But it is also important to understand the degree to which the elevated incidence of chronic health disorders can be attributed to conditions that arose secondary to the original work-related injury or illness.”
Research questions to come
As the team conducts follow-up interviews at the 36-month post-injury mark, researchers have already begun using this dataset to conduct other studies. One is on patterns of cannabis use to treat post-injury health conditions. Another is on predictors of persistent pain. Yet another examines the links between injured workers’ interactions with WSIB case managers and the likelihood of developing a mental health disorder.
Several other studies are focused on RTW practices. “We want to know more about what it is in a workplace that predicts the offer of modified duties and accommodations, and the quality of the accommodations offered,” said Mustard. “We also want to identify the characteristics of workers, workplaces and sectors that predict a successful return to work.” The team is also looking at differences in RTW practices at the workplace level across 10 economic sectors (from which enough participants were recruited to allow for comparison).
To watch Mustard’s webinar, go to: www.iwh.on.ca/events/speaker-series/2021-feb-02. New findings from this research project will be posted, as they become available, on the project page: www.iwh.on.ca/projects/ontario-life-after-work-injury-study.