Although the COVID-19 virus still lingers among the population, many workplaces have removed mask mandates and taken down plexiglass dividers. But looking back on the height of pandemic—with waves of rising and falling case counts, workplace outbreaks and work-from-home protocols in full swing—it’s clear that workplaces were a key setting for a proportion of COVID-19 transmission.
But what proportion? That’s a question not easily answered, given the dearth of data about work exposures during the pandemic. A new study led by Dr. Peter Smith, president and senior scientist at the Institute for Work & Health (IWH), took a retroactive look at the first two years and five major waves of the pandemic, to paint a picture of trends in work-related COVID-19 infections in Ontario.
The research team found that, between April 1, 2020, and April 30, 2022, the risk of work-related COVID-19 infections changed from wave to wave. Importantly, it did not mirror the changes in risk of getting COVID-19 in the general working population. Further, certain workplace factors—including working close to others, working indoors and having a public-facing job—were associated with an increased risk of getting an infection, as would be expected. But the strength of this association also varied across the different waves of the pandemic.
To take an example, working in close proximity with others carried much lower risk in wave three than in wave one, but higher again in wave five. The dynamic nature of this and other work exposures was something we found and were surprised by,
says Smith, whose paper about this study was published in February 2024, in the journal Occupational and Environmental Medicine (doi:10.1136/oemed-2023-109243), part of the BMJ publishing group.
This tells us that something was altering the risk of work-related transmission at different points in the pandemic. And that something may potentially be changes within workplaces, such as the presence of, or adherence to, different infection control practices,
says Smith.
But to pin down exactly what factors were driving that change in risk—particularly to better target prevention efforts in real time—this sort of workplace transmission data should have been collected much earlier in the pandemic,
he notes.
How the study was done
To determine how many COVID-19 cases in Ontario were work-related, the research team used workers’ compensation claims data from the Ontario Workplace Safety & Insurance Board (WSIB). Smith notes that compensation claims data do not cover every single work-related infection that occurred–such as when a workplace isn’t insured by WSIB, a work-related COVID-19 claim is not accepted, or someone does not submit a claim for a work-related infection. But he adds that the accepted claims for COVID-19 within this dataset were assessed by WSIB and can confidently be classified as work-related.
The researchers then combined the accepted claims data with data from Statistics Canada’s Labour Force Survey, which in April 2020 added questions to understand the impacts of the pandemic, such as whether respondents worked most often at home or at the workplace. The Labour Force Survey data allowed the researchers to better estimate the population at risk of work-related COVID-19 infections by using data of only those who mostly worked at the workplace or outside of their home. One of the key challenges in determining the rates of work-related COVID-19 cases was the dramatic shift to remote work for a large proportion of the working population. This meant that using historic data, such as census data from 2016, was not going to provide an accurate reflection of the number of people who may have been exposed to COVID-19 at work,
Smith explains.
Finally, the research team used a job exposure matrix to estimate the role certain workplace factors may have played in increasing the risk of infection. This job exposure matrix was previously developed by researchers in the U.S. to broadly classify occupations as having different types of working conditions. The team used this classification system to identify whether workers with COVID-19 claims were working under three conditions (or exposures): worked in close proximity to others, worked indoors and had a public facing job.
What the study found
To identify rates of work-related COVID-19 infections, the research team examined the number of claims that occurred per 1,000 full-time equivalents (FTEs; an FTE is equivalent to a 37.5-hour work week). They combined the compensation claims data with data from the Labour Force Survey to account for the month of the claim, the presence of any of the three occupational exposures, age, sex and industry. The rate of work-related COVID-19 infections changed over the course of the five waves, being highest in the fifth wave, and lowest in the third wave.
| COVID-19 Wave | Time Period | Rate of work-related COVID-19 infections (claims per 1,000 FTEs) |
| 1 | April 2020 to August 2020 | 10.11 |
| 2 | September 2020 to February 2021 | 17.65 |
| 3 (Alpha) | March 2021 to June 2021 | 14.51 |
| 4 (Delta) | July 2021 to November 2021 | 1.91 |
| 5 (Omicron) | December 2021 to April 2022 | 26.41 |
The risks also differed between work-related COVID-19 infections and overall COVID-19 cases among the entire working-age population in Ontario. The rate of work-related COVID-19 cases in wave four was a fifth of the rate seen in wave one, whereas the rate of overall cases in wave four was twice as high as in wave one. Rates of work-related cases during the fifth wave were just over 2.5 times as high as they were in wave one; in contrast, rates of overall cases in the fifth wave were more than 18 times as high than in the first wave.
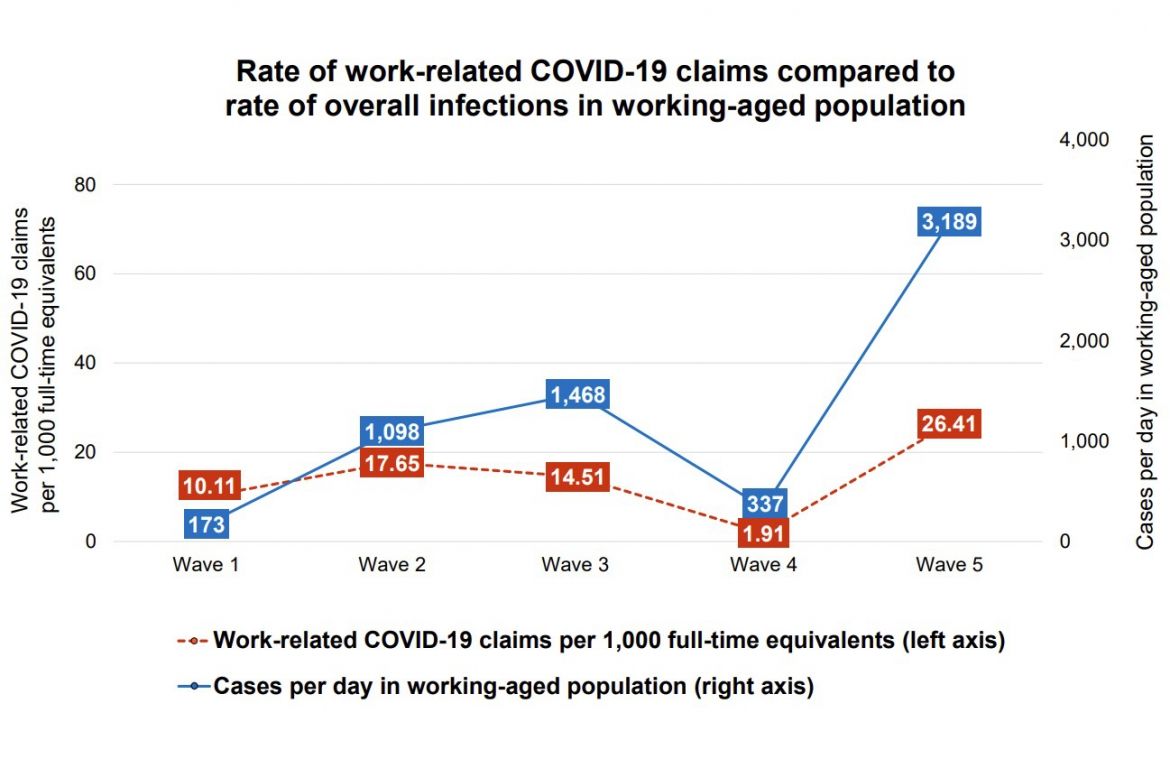
Finally, the three occupational exposures were all associated with an increased risk of work-related COVID-19 infections. The risk was almost three times as high for those working in close proximity to others (compared to those not in close proximity); 79 per cent to 90 per cent higher for those working primarily indoors (compared to those working primarily outdoors); and 30 per cent higher for those with a public facing job. However, this association changed throughout the pandemic, being markedly stronger in the first and fifth waves of the pandemic (with the exception of public facing occupations), and weakest in the third wave. This means that in the first and fifth waves, for example, having a job that required someone to work indoors or close to others increased that person’s risk of infection more than in other waves of the pandemic.
Such findings raise several questions, notes Smith. What might have been behind the less dramatic change in rates of work-related infections from wave to wave (compared to the change seen in cases for the working-age population), as well as the changing risks associated with workplace factors?
he asks. The answers may be that infection control measures in the workplace were executed better than in other aspects of daily life—but we don’t have the data to determine this for sure,
he adds.
As Smith notes, one of the main messages from these findings is the need for better data collection in the future. When it comes to estimating workplace COVID-19 exposure, worker’s compensation claims are not without their faults,
he says. However, the fact that the changes in work-related infections over time were not the same as the changes in overall infections among the working-aged population tells us that using overall infections in the general population as a whole as a proxy for work-related infections would likely introduce potentially important errors.
To have a better system for estimating work-related infections in future pandemics, and in a more timely manner, we need to routinely collect and integrate the collection of work information with health data,
says Smith. He adds that this data would also be helpful in investigating other occupational health concerns. There are going to be both financial and resource costs to do so, but the costs of not doing it are likely greater because we will be making decisions on incomplete or even incorrect information.